What is Malassezia dermatitis in dogs?
Fungi of the genus Malassezia were first identified by the scientist Louis Charles Malassez in 1904, which is how they got their name. Later they were reclassified into two types. Some are found on human skin, while others are found on animal skin.
Did you know? The drinking technique is the same for dogs and cats. They bend the tip of the tongue, form a groove and lift liquid to the mouth of the throat.
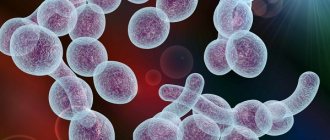
Malassezia yeasts are distinguished by a thick cell wall consisting of many layers. They reproduce in repeating buds. The species Malassezia pachydermatis grows well in a lipid-free environment, but if they are added, growth is enhanced. Lipid-dependent types of fungus can be observed in cats. Dogs are always colonized by the pachydermatis species.
Malassezia pachydermatis lives on the mucous surfaces and skin of dogs. More often it occurs in places with increased secretion from the sebaceous glands, as well as in the ear, chin, skin folds, between the fingers, mouth, rectum, vagina, and paraanal glands. The fungus is often associated with otitis externa in dogs. When analyzing healthy animals, the fungus was detected in the lip area in 80%, in the folds between the fingers in 60%, in the mucous membrane in 53%, and in the ear canal in 33%. For dogs with Malassezia dermatitis, the quantitative colonization of the fungus, compared to healthy animals, increases by 100–10 thousand times.
Causes of ear fungus
Once again, the fungus will not “break through” the immunity of a healthy cat. In cases of fungal pathologies, you always need to think about what exactly was the root cause:
- Allergic reactions.
- Parasitic infestations.
- Diseases of bacterial etiology.
- Foreign bodies entering the ear canal.
- Injuries.
- Anatomical factors (for example, congenital anomalies of the ear canals).
- Hereditary pathologies that reduce immunity.
- Diseases of the endocrine glands.
Finally, we should not forget about long-term use of antibiotics or corticosteroids, but we have already written about them above.
Characteristics of predisposing factors
Allergic reactions. Allergies very often contribute to the appearance of fungal pathologies. Moreover, sometimes “fungal” inflammation in the ears appears even before the first signs of allergy appear. There are two problems here: firstly, allergic reactions themselves greatly weaken the immune response (since the body is busy destroying itself). Secondly, with these pathologies, the environment inside the ears changes significantly, which also has a beneficial effect on the growth and development of fungi (and yeast in particular)
Why does the disease develop?
Malossezia does not cause skin diseases unless certain conditions are created that promote its development. The conditions that favor the transition of a fungus from a normal microorganism to a pathogenic state have not been sufficiently studied by scientists.
Did you know? Dogs can sense how much time has passed. They may react differently when their owners are away from home for different periods of time.
Most likely, this is facilitated by various kinds of disorders of the body, which normally control microbial colonization. Such disorders may be physical, chemical or immunological in nature. For Malassezia dermatitis to occur, predisposing factors must be present.
Decreased immunity
Immunodeficiency is a possible cause of the disease. Immunoprotective mechanisms normally limit the excessive colonization of the skin by microbes. But if they are violated, the pathogenic development of the fungus increases.
Improper care and living conditions
Frequent bathing of the animal increases the moisture content of its skin. This promotes the development of fungus. Improper care of animals with skin folds or floppy ears can also lead to its development. Malossezia develops on skin whose pH is in the range of 4–8.
The skin of dogs has the highest pH among mammals. This figure may vary depending on the breed. More alkaline skin is more susceptible to infections than acidic skin. High pH levels in dog shampoos can cause irritation if there are skin problems.
Chronic diseases
A number of diseases lead to the development of fungus: food allergies, endocrine diseases, dermatitis, keratinization, viral leukemia. The relationship between various diseases, infections and fungal growth is not well understood. But treating the disease can sometimes prevent its development or reduce its manifestation.
Important! If an increased proliferation of staphylococci is observed on the skin of an animal, this provokes the development of yeast fungi, since the species are in a symbiotic relationship.
Other reasons
The prevalence of the disease is influenced by the climate of the area. High ambient temperatures with high humidity favorably affect the growth of the fungus, while dry weather conditions prevent this process. An increase in ambient temperature in summer and spring leads to increased sweating, which can trigger the development of the disease.
What dog breeds are predisposed to Malassezia?
There is no predisposition of an animal to Malossezia depending on age and gender. But there are breeds in which the disease appears more often. Among them it is worth highlighting: basset hound, Scottish and Australian terriers, cocker spaniel, dachshund, miniature poodle, shih tzu.
annotation
The genus consists of 14 Malassezia
of yeast-like fungi, 13 of which are lipophilic and 1 is non-lipophilic.
They are commensals and in predisposed individuals they usually cause a range of chronic, recurrent infections. In rare cases, they cause such serious diseases as infections that occur during vascular catheterization, during hemodialysis, and can cause peritonitis, etc. Although these mushrooms have been known to mankind for more than 150 years, due to the whimsical nature of mushrooms, their bulky cultures, and the ability to speciate, they have not been sufficiently studied. Since the last taxonomic revision, 7 new species have been added to this genus. Their ability to evade host immunity and increase in virulence, the range of diseases they cause has increased. Recently, Malassezia
have been implicated as a causative agent in the common disease atopic dermatitis. Although research on fungal cultures is complex, new molecular analysis techniques and advances in instrumentation have prompted an increase in research in this area. Therefore, we can pay more attention to this type of fungi to study in detail their characteristics and their growing impact on the disease clinic.
What was known?
Malassezia
causes superficial mycoses, but systemic infections are rare. They do not have descriptions of drug resistance.
Introduction
Malassezia
(formerly known as Pityrosporum) forms a cutaneous synanthropic flora that is associated with a variety of clinical manifestations, ranging from benign skin diseases such as pityriasis versicolor to hematogenous fungal infection in the immunocompromised individual.[1]
Currently, 14 species have been described, namely Malassezia furfur
,
Malassezia pachydermatis
,
Malassezia sympodialis
,
Malassezia globosa
,
Malassezia
o
btusa
,
Malassezia restricta
,
Malassezia slooffiae
,
Malassezia equina
Malassezia dermatis
, Malassezia japonica
, Malassezia nana
,
Malassezia capre
,
Malassezia yamatoensis
, recently
Malassezia cuniculi
was discovered .[2] Due to their lipophilic nature, these fungi are able to colonize seborrheic areas of the skin and survive on the fatty acids normally present in sebum.
They cause the following skin diseases: hyperkeratosis, invasion of hair follicles and inflammation. Although, by definition, superficial mycoses do not extend beyond the horny epithelium, these fungi are detected in the mouth, central and deep layer of the hair follicle. Malassezia
infections can be superficial and localized, and can also be systemic in immunocompromised people.[3]
Spread on skin
Malassezia skin colonization density
depends on age, body area and comorbid skin conditions, as well as on the person’s place of residence.
Being lipophilic, the highest prevalence of Malassezia
is found in sebaceous areas of the skin such as the scalp, face and upper torso.
Malassezia
most often found in younger people, who tend to have oilier skin.[3]
Factors affecting the reproduction of Malassezia
Geographical factor: depending on the geographical area, the density of different species of the genus Malassezia
on the skin.
The most favorable zones for the growth of Malassezia
are subtropical and tropical climates.
Research shows that the growth of Malassezia globosa
increases during the summer when temperatures are high and sweating is increased.[4]
Age factor: pityriasis versicolor affects people from 20 to 40 years old. However, in India, it is seen in people in the age group of 10 to 30 years. Pityriasis versicolor is rare in children and the elderly. [5,6,7,8]
Hormonal factor: corticosteroid therapy, malnutrition, increased serum cortisol concentrations contribute to the occurrence of pityriasis versicolor in patients.[9]
Pathogenesis: Human sebum, which is a complex mixture of lipids, is the source of nutrition for this type of yeast. Sebum consists of triglycerides of fatty acids, waxes, esters, sterol esters, cholesterol, cholesteryl esters and squalene. Sebum is utilized by breaking down triglycerides and esters into diglycerides, monoglycerides and free fatty acids. Thus, changes in the secretion of sebum and its breakdown causes the development of dandruff. Malassezia infection
, is also associated with increased sweating.[10
a
,
b
,11,12,13]
Clinical scenarios
Yeast of the genus Malassezia
cause the development of chronic recurrent dermatoses such as pityriasis versicolor, seborrheic dermatitis and folliculitis.
Malassezia
has recently been shown to play a role in the pathogenesis of atopic dermatitis and psoriasis, especially in cases involving the scalp.
In addition, studies mention Malassezia
, which is the causative agent of confluent reticular papillomatosis and onychomycosis.
This yeast is also associated with catheter-associated infections among neonates receiving total parenteral nutrition and in frail older adults receiving parenteral lipid supplements. Also, such patients may experience hematogenous fungal infection and sepsis caused by Malassezia furfur
and
Malassezia pachydermatis
.[1,14]
Pityriasis versicolor
Malassezia infection
.
Pityriasis versicolor, also known as pityriasis versicolor, is a common superficial mycosis that is a chronically recurring infection of the stratum corneum of the skin. It is characterized by small white scales, hypo- or hyperpigmented macules, which are unevenly distributed throughout the body and are most often found on oily areas of the skin on both the trunk and extremities. Some patients may experience itching, but most patients are asymptomatic.[1] The Latin name for pityriasis versicolor (or multicolored) is pityriasis versicolor
.
It comes from the Greek. “ P ityron
” - “flakes, scales.”[3,15]
Back in 1871 Neumann
et al.[16]
revealed that it is the mycelial forms of Malassezia
that are responsible for the appearance of pityriasis versicolor.
Successful cultivation of Malassezia
is described in the works
of Neumann
et al.
and Gordon
et al.[17]. It was also found that yeast forms can be seen both on areas of skin affected by pityriasis versicolor and on healthy areas of skin. It was found that in order for the clinical picture of pityriasis versicolor to manifest itself, the necessary conditions are a large proliferation of fungal filaments, and they must secrete several serovar A antigens.[1]
Differential diagnosis
Skin lesions caused by pityriasis alba, pityriasis rosea, vitiligo, hypopigmented mycosis fungoides, erythrasma and seborrheic dermatitis look similar.
Diagnosis
Pityriasis versicolor is diagnosed clinically; only in rare cases is a biopsy or Malassezia
. Under a Wood's lamp, pityriasis versicolor fluoresces yellow. Examination of mushrooms with 10% potassium hydroxide solution shows single-celled, short, curved, straight mycelium filaments and spore clusters. All of the above should resemble “meatballs and spaghetti.”
Histopathological examination
Although pityriasis versicolor is rarely biopsied, it has spores (yeast form) and short hyphae (mycelium) in the stratum corneum of the skin, which are detected using diazonium blue, periodic acid-Schiff, or silver nitrate-methenamine complex. Moderate hyperkeratosis and acanthosis are rare.[3]
Malassezia species that do not cause pityriasis versicolor
Pityriasis versicolor is caused by several species of Malassezia
[18,19,20,21],
M. globosa
is the most common causative agent of lichen with a probability of 58.2%, 55%, 55% and 53.3%, respectively.
A study conducted in north central India found 54% M. globosa
, and 30%
M. furfur
.
Several studies have shown that M. furfur
predominantly causes pityriasis versicolor.
Makimura
et al.
identified M. furfur
and
M. sympodialis
in temperate climates;
however, in tropical countries, they isolated M. globosa
.[22,23,24]
Pathogenicity of M. globosa
due to its esterase and lipolytic activity. Unlike other mycoses, here, in the center of the lesions there are more viable cultures.[25]
Seborrheic dermatitis
Seborrheic dermatitis is the second most common infection associated with Malassezia
, which was originally described by
Unna PG
in 1887. It is a superficial eczematous dermatitis, can be subacute or chronic, and is characterized by the presence of an erythematous plaque with dry or greasy scales. It is found in areas of the skin rich in sebaceous glands, such as the scalp, face, ears, chest and armpits. Weak corticosteroid drugs have proven effective in treatment.
However, the relapsing nature of this disease makes it difficult to treat. Antifungal therapy should be the mainstay in the treatment of this disease, since the use of corticosteroids does not reduce the number of Malassezia
.[3,26]
Seborrheic dermatitis is common during periods of a person's life when their glands are most active:[15]
- First 3 months of life (infantile seborrheic dermatitis)
- During puberty
- When sebum production declines after age 50.[15]
This disease affects 3-5% of the population, with more men than women. In immunocompetent individuals, seborrheic dermatitis usually begins during periods of high sebum secretion, i.e. during puberty and become chronic and recurrent forms. Stress is known to aggravate this type of dermatitis. In patients with AIDS, resistance to antifungal therapy for seborrheic dermatitis is observed from 30 to 80%, in contrast to immunocompetent individuals. [27]
In HIV-infected patients, the appearance of seborrheic dermatitis is a surrogate marker of CD
4+ T lymphocytes.
M.
restricta
and
M. globosa
are observed primarily on the scalp, both during health and illness.[28]
Pathogenesis
The immunopathogenesis of seborrheic dermatitis is complex and multifactorial.
It has been proven that the increased density of colonies is higher in damaged skin than in undamaged skin. However, techniques must be standardized to prove this. Recently, “quorum sensing”—the ability of some organisms to communicate and coordinate their behavior through the secretion of molecular signals—has been actively discussed in science. Malassezia
also operates according to the “quorum” principle.
Also Malassezia
has a complex antigenic structure, represented by both protein and carbohydrate antigens, which are associated with the stages of their life cycle;
protein antigens appear in the early stages of growth and are associated with the development of cell walls and cytoplasmic organelles, while carbohydrate antigens are derived from mannan and mannoproteins. Research by B ergbrant
et al.
showed an increase in NK
cells, impaired T cell function in addition to an increase in total serum
IgA
and IgG among
patients
with seborrheic dermatitis.
However, the titer of Malassezia
-specific antibodies was not elevated, so it was suggested that hypergammaglobulinemia may occur as a reaction to toxins contained in yeast and to lipases.
People suffering from dandruff have loosely connected corneocytes or a small number of dysmosomes. The level of secreted lipids is reduced, which in turn affects the epidermal water barrier. Itching associated with histamine also increases, causing damage and reducing the effectiveness of the skin's defense mechanism. All this makes it easier for Malassezia
into the skin.
Malassezia
produces lipases that break down sebum into arachidonic and oleic acids, which are irritants and have a desquamative effect on keratinocytes. Thus, this contributes to the onset of the inflammatory process and creates vicious circles.
In some cases Malasseziae
have the ability to exist as pathogenic microorganisms that cause seborrheic dermatitis, and in other cases exist as normal flora. They are capable of causing an immune response. They activate the classical and alternative pathways of the complement cascade. Complement component C3 has been found in damaged skin and has been postulated as one of the causes of inflammatory reactions. Although yeast should ideally be phagocytosed and eliminated by our immune system, it is capable of suppressing the secretion of cytokines and interleukins.
Malassezia
alters and evades the local immune response by producing secondary metabolites that contribute to seborrheic dermatitis.[28] Environmental factors, stress, UV radiation, climate change, hormonal changes and trauma also likely contribute to the maintenance of seborrheic dermatitis.[28]
Milky crusts: Infantile or neonatal seborrheic dermatitis is also called pityriasis capitis, which is a nonpruritic dermatosis ( Cradle
cap directory
,
WebMD
.
Retrieved
August
26 , 2012).
Infantile seborrheic dermatitis usually occurs from the 2nd week of life to 6 months. The rashes can be eczematous and psoriasis-like in nature, rare localizations of seborrheic dermatitis are the face, torso and sternum area. The lesions can be single or multiple, and can merge, especially on the face in the fold area.[15]
Neonatal cephalic pustulosis (neonatal acne)
A child has skin colonization with Malassezia
begins on the first day of life.
Malassezia
is transmitted to the baby from the mother and from health care workers, and colonization increases during the first weeks of life.
Environmental factors and maternal hormonal levels influence the colonization process. The high prevalence of M. sympodialis
in newborns is observed from birth and is the cause of neonatal acne.[29]
Folliculitis caused by Malassezia
Synonyms: pityrosporum folliculitis.
This intensely pruritic, follicular papulopustular rash is seen usually on the upper torso in the young age group and is rare in older people.
This disease was first described in 1969 by Weary
etal., based on the histological ultrastructure
of Potter
etal. in 1973 it was discovered that it was a separate type of disease. This is a chronic infection in which patients typically present with erythema, papules and pustules on the chest or back, and a follicular pattern. The distinctive symptom is itching. Rare localizations are the face, neck, shoulders and arms.[6,15,30,31]
Risk factors for folliculitis:[32,33,34,35,36,37]
- Immunosuppression
- Diabetes
- Broad-spectrum antibiotics
- Steroids
- Puberty,
- Pregnancy
- Cosmetics, lotions, sunscreens, emollients, olive oil, which are the cause of skin clogging.
Diagnosis: The diagnosis of folliculitis is based on the clinical picture and positive response to antifungal therapy.
Some differences in the distribution of Malassezia
according to epidemiological data:
Low number of Malassezia
, compared to normal skin, causes other diseases.
There are pathogenic strains that are not isolated in psoriasis.
Histopathological findings: According to microscopy, the discharge from the pustules represents budding yeast forms and spores, and not hyphae, as in the study of pityriasis versicolor. to diagnose pityrosporum
folliculitis
, but histology shows dilated hair follicle openings with large amounts of cellular material and keratin plugs.
The inflammatory response is caused by lymphocytes, histiocytes and neutrophils. The mouth of the sebaceous gland ducts is surrounded by monocytes and mucin deposits. Yeasts of the genus Malassezia
can be detected in hair follicles; however, they are more often found in the orifices of the sebaceous gland ducts. Periodic acid-Schiff and Grocott-Gomori staining can be used to identify unipolar budding yeast cells; mycelial forms were not detected by these methods. [38],[39],[40]
Treatment
Treatment for pityrosporum
follicilitis
uses oral antifungal medications, since topical medications do not penetrate the hair follicles. Since there is a high relapse rate, there is a need for maintenance therapy.
Atopic eczema/dermatitis syndrome
Atopic dermatitis is a chronic, inflammatory skin disease. Patients with atopic dermatitis often have bronchial asthma. The pathogenesis is not entirely clear. Patients suffer from itching, which may be the body's response to irritants or microorganisms, due to the loss of surface barrier mechanisms in dry skin [Fig. 1]. [3],[41],[42]
Rice. 1: Malassezia
in the pathogenesis of atopic eczema/dermatitis syndrome
After the successful therapeutic use of ketocanazole in the treatment of atopic dermatitis, a number of studies have proven the role of Malassezia
as one of the etiological factors in the occurrence of exacerbation of atopic dermatitis. [43]
Their multilayer membranes and cell wall mannans contain antigens. of Malassezia among patients
-specific
IgE
, and they have positive skin prick tests.
Malassezia
may act as a persistent allergic irritant.
The combined cellular and humoral immune response leads to increased sensitization. The cellular response leads to the activation of T h
2 lymphocytes, this leads to an increase in the levels of IL 4 and IL5 compared to the control group of healthy people.
Due to allergen-specific IgE
and cytokines release histamine from mast cells.
Symptoms of itching due to histamine release lead to further sensitization of Malassezia
.
Antifungal drugs lead to a decrease in the yeast population on the skin, thereby reducing the antigenic load, which prevents the inflammatory process.
IgE
specific are determined to
M. sympodialis
,
M. furfur
and, more recently, to
M. globosa
.
Isolation and speciation
Several studies have been conducted on M. globosa
,
M. restricta
,
M. sympodialis
and
M. furfur
.
M. globosa
the allergen is responsible for the production of heat shock protein 70.
In 2002 Sugita
et al.
described new species
of
M. dermatis
isolated from patients with atopic dermatitis in Japan.
However, the researchers suggest that more studies should be conducted in other countries as well to confirm the fact
that
M. dermatis
can be detected in patients with atopic dermatitis not only in Japan.
The pathogenesis of the disease is not very clear. Genus Malassezia
promotes the production of
IgE
-specific antibodies, and this plays an important role in pathogenesis.
More research is needed to understand the role of Malassezia
in the mechanisms of disease, chronicity and exacerbation. [3],[15],[41],[42],[43],[44],[45],[46],[47],[48],[49],[50],[51 ],[52]
Psoriasis
It has been documented that chronic plaque psoriasis and psoriasis vulgaris are caused and aggravated by Malassezia
.
Rivolta
et al.
in 1873 he first proved this fact. Later, in 2007, Narang
et al. [53] treatment with fluconozole is effective for psoriasis.
Among patients with psoriasis, especially those whose affected area involves the scalp, eyebrows, ears, and trunk Malassezia
plays a big role.
Elewski
et al.
in 1990 [54] reported a case of guttate psoriasis in areas affected by Malassezia folliculitis
.
Some differences have been noted in the epidemiological data and distribution of the genus Malassezia
.
The pathogenesis is not fully understood. Triggers of T cell activation and cytokine release are multifactorial - stress, infections, trauma, drug use, etc.
Autoantigens: 13 keratin has homology to K17, which is an identified candidate autoantigen that is not normally found in adults but appears in response to injury.
This explains the Koebner phenomenon, where new lesions appear at sites of injury. Neutrophils are found in psoriasis in the skin infiltrate and increase chemotoxic reactions.
This phenomenon does not occur when the skin is damaged by staphylococci.
Superantigens are those antigens that cause a cytokine storm. Superantigens are staphylococci and streptococci, which aggravate the course of atopic dermatitis, guttate psoriasis and chronic psoriatic plaques.
It can be said that the superantigen promotes inflammation by activating complement, producing inflammatory cytokines and recruiting neutrophils, but this fact is not fully proven.
Malassezia colonies
on skin affected by psoriasis may be due to the fact that keratinocytes produce antimicrobial peptides.
These peptides destroy the normal bacterial microbiota in the affected area and allow only selective overgrowth of Malassezia
.
This proliferation itself promotes an increase in the number of keratinocytes and an increase in the level of LL
37 (human cationic antimicrobial protein).
This can cause the development of psoriatic rashes. However, the number of colonies is always lower compared to the healthy control group. The reason for this is not very clear, but may be due to the inhibitory effect of LL
37 noted in patients with psoriasis.[3,15,55]
Indirubin, an indole produced by Malassezia
, have been successfully used in treatment, further strengthening the association
of Malassezia
with this disease.[3,15,55,56]
Onychomycosis
In Malassezia
there are no enzymes with keratolytic activity.
They are lipophilic and so nails are not a good source of lipids, there are no lipids under the nail plate, Malassezia
does not colonize them.
Malassezia
is not considered to be the primary causative agent of onychomycosis.[2,56]
Table 1. Diseases rarely caused by Malassezia
.
Superficial infections | Deep infections |
| Confluent reticular papillomatosis | Mastitis[61] |
| Dacrocystitis[57] | Sinusitis[62] |
| Vulgar acne[58, 59] | Septic arthritis[63] |
| Seborrheic blepharitis[59, 60] | Malignant otitis externa[64] |
| Nodular hair infection |
The role of Malassezia in the occurrence of systemic diseases
There have been reports of a role for Malassezia
as an infectious agent during peritoneal dialysis in a patient with chronic renal failure.
Several cases have been reported implicating Malassezia
in the development of peritonitis.
Hassal
et al.
notes pulmonary embolism and pulmonary infection due to Malassezia
in a patient who was on urokinase therapy.
Role of Malassezia in catheter-associated blood infections
Catheter-associated sepsis due to Malassezia
, was found in low birth weight infants and in intensive care unit patients who were on total parenteral nutrition and in those with predisposing conditions.
two
species, namely M. furfur
and
M. pachydermatis
are proven causative agents of systemic disease.[65,66,67,68,69,70,71,72,73]
Involvement of Malassezia pachydermatis in the development of human infections
This species was isolated in 1925 by Weidman
from a captured Indian rhinoceros.
He named it pityrosporum pachydermatis
. [74]
Dodge
et al.
in 1935 assigned it to the genus Malassezia
. This species exists as normal flora in domestic animals such as dogs, cats, and also in wild animals. Skin colonization is common among pet owners
For the first time M. pachydermatis
was described in 1983 as a causative agent of peritonitis during peritoneal dialysis in a patient with insulin-dependent diabetes.
M. pachydermatis
was the cause of a hematogenous fungal infection in the neonatal intensive care unit in 8 low birth weight preterm infants receiving total parenteral nutrition with lipid supplements.
M. pachydermatis
was isolated from the blood of 6 of 8 newborns, from the tracheal aspirate of 2 of 8, from the eyes of 1 of 8, from nasal secretions in 1 of 8, and from urine in 1 of 8 newborns.[75]
M. pachydermatis
may lead to outbreaks as it can persist on the surface of the incubator for up to 3 months, despite standard disinfection.
Thus, the following were implemented: careful personal hygiene of medical and neonatal care personnel, as well as modifications to cleaning procedures.[72] Colonization of pet owners by Malassezia
was demonstrated by high rates of amplified DNA compared to those who did not own pets.
Thus, M. pachydermatis
is a potential pathogen.[15]
Malassezia
pachydermatis
was isolated from a facial granuloma in a healthy woman and her dog from skin scrapings and earwax. The skin lesions healed after oral fluconazole and cryotherapy.
conclusions
Genus Malassezia
known to mankind for more than 150 years as a synanthropic group of opportunistic fungi.
Although they are generally not life-threatening, causing only chronically recurring superficial mycoses in most cases, this fact is taken into account when searching for the causes of a wide range of diseases, including systemic infections. It is a potential pathogen among predisposed patients and among patients receiving intensive care. The taxonomy of Malassezia
has been supplemented with 7 new species. More research is needed to understand their behavior in clinical settings. The minimum inhibitory concentration of antifungal drugs used against newly identified species should also be studied.
What's new?
New relationship between pathogens and diseases such as atopic dermatitis and psoriasis, etc.
Documentation of high minimum inhibitory concentrations obliges us to understand the spectrum of diseases caused by the genus Malassezia
, including knowledge of rare diseases caused by these pathogens.
How do symptoms appear?
Skin lesions can be observed in one place or scattered. They are mainly found on the animal's face, the front of the neck, in the external auditory canal, in the axillary fossae, groin area, interdigital folds or in areas with diaper rash. Symptoms of the disease include redness of the skin, partial or complete baldness in the affected areas, scaliness or excessive fatty discharge.
Important! The fungus Malassezia pachydermatis is not transmitted to humans.
In chronic cases, thickening of the skin is observed as a secondary element of the rash, increased skin pattern, and impaired pigmentation of the affected area. Itching of the skin can be of varying degrees. The disease is distinguished by a specific skin odor and brown discharge from the ear canal. The animal's claws also turn brown.
Prevention
Let's summarize. Firstly, Malassezia in cats is caused by yeast fungi, which are not initially pathogenic. The main symptoms are hair loss and skin irritation, which is often mistaken for an allergy. Secondly, an accurate diagnosis can often be made not only on the basis of microscopic examination, but also by the animal’s response to treatment. How can you prevent the occurrence of this disease?
Of course, there is no specific prevention, but some advice can still be given. Firstly, if your cat is suffering from some kind of infection, do not delay its treatment under any circumstances! Secondly, for seborrhea, be sure to use special washing shampoos, and do not be lazy to do this more often. Thirdly, do not hesitate to seek help from a veterinarian whenever something bothers you about your pet’s behavior or appearance.
How is the diagnosis carried out?
To identify the fungus Malassezia pachydermatis, various diagnostic methods are used. These include cytological, pathological tests and culture. Cytological examination makes it possible to quickly determine the presence of the fungus. To do this, transparent tape is glued to the affected skin and then removed. The sample taken is subject to special staining and examined under a microscope with a magnification power of one hundred times. If the fungus is easily established, it is concluded that the skin is infected. In case of single detections, the analysis is considered to have given a negative result. Dry scrapings and smears are alternative cytological methods.
To quantify the fungus, a method using Petri dishes is used for diagnosis. The fungus is cultivated in small dishes with a special propagation medium, applying it to the affected area for 11 seconds. For 4–7 days at a temperature of 32–37°C, conditions are created for growing the mushroom. The result indicates the density of the fungal population. It is interpreted taking into account the location of the infected area on the animal’s body and the breed of the dog.
Important! Using a biopsy, you can see the fungus in the dry affected layer of skin. Histological sections do not always give reliable results.
How to treat Malassezia in dogs
Treatment of dogs with Malassezia dermatitis involves treating the affected areas of the skin and systemic use of medications at home. The goal of this therapy is to reduce the amount of Malassezia fungus and bacteria on the skin. It is also important to correct existing diseases that contributed to the development of the infection. Since the fungus is localized in the stratum corneum, local therapy gives a positive result. In addition, it relieves unpleasant odor and discharge in severe forms. For otitis, drops are prescribed in the ear. Antifungal ointments, sprays, gels are applied to the affected area. Medicines in tablet form are given orally as prescribed by the doctor.
Antifungal therapy provides a number of rules:
- the affected area should be cleaned before applying the drug;
- observe the dose and number of treatments;
- Give oral medications according to the dosage and do not interrupt treatment prematurely.
Necessary drugs
Therapy is selected individually by the doctor. Prescriptions depend on the severity of the disease, localization and distribution of the affected areas. Animals must be treated comprehensively. Therefore, the use of drugs, treatment of affected areas, and specific antibiotic therapy should be used.
Did you know? A dog's whiskers detect even the slightest change in air currents. Therefore, they help her sense danger even in the dark. Sweat glands in dogs are located only between the pads of their paws. Therefore, the cooling system for animals is their breathing.
The following have an effective effect on the pet’s body:
- Shampoo with 2% miconazole and chloghexadine. This product degreases the skin well and has antibacterial and antifungal effects. Washing the animal should be done every three days for 3 weeks.
- Other forms of local action (drops, creams, ointments) containing selenium sulfide, enilconazole, chlorhexadine, benzene peroxide, azole are widely used in the treatment of Malassezia.
- A solution of 2–3% vinegar. Prescribed as an additional treatment for treating affected areas. This substance changes the acid-base balance of the skin towards acidification and creates unfavorable conditions for the development of the fungus.
- An antibacterial agent for external use can be prescribed lime sulfur.
- Systemic treatment. It is prescribed in severe cases, or when the owner is unable to bathe the pet frequently. Typically this is ketoconazole orally at a dose of 2.5–10 mg per 1 kg of body weight twice a day for 7–15 days. This medicine may cause severe hepatotoxic reactions. Itraconazole (5 mg/1 kg body weight, once daily) is better tolerated by dogs.
Antibacterial therapy is combined with the prescription of local drugs that do not fight bacteria. The duration of treatment is 2–4 weeks. If antifungal therapy does not produce positive results, the doctor considers concomitant diseases and prescribes treatment based on this. There are cases when the cause of the disease is not clear. Then maintenance treatment is carried out for life. For this purpose, ointments, creams and shampoos with ketoconazole are used.
How is Malassezia pachydermatis treated?
The dosage of antifungal agents is different for animals and humans. The treatment regimen is determined by the veterinarian; self-medication can aggravate the condition. Treatment for Malassezia in cats includes antifungal medications such as:
- "Ketoconazole";
- "Itraconazole";
- "Chlorhexidine";
- solution of sulfur and salicylic acid;
- piroctone olamine;
- selenium sulfide;
- "Enilconazole".
Before starting antifungal therapy, it is necessary to cure the concomitant ailments that caused Malassezia.
You can increase your cat’s immunity with vitamin complexes:
- "Canvit Multi";
- "Kanvit Nutrimin";
- "Natur Protection Daily Vitamin Formula";
- "Beafar."
Balancing your diet will help speed up the healing process. A balanced diet with medicinal food is also recommended to restore the structure of the coat and skin. These include:
- Royal Canin Intense Beauty;
- "About Plan Derma Plus";
- "Brit Car Kat Sunny Beautyful Hair";
- "Trainer Staff Adult Beauty."